The parasite harms the lymph system in our body, most contaminated individuals have no side effects and won't ever give clinical indications. These individuals don't realize they have lymphatic filariasis until it will investigate. A little level of people will experience lymphedema. This is brought about by liquid assortment on account of the inappropriate working of the lymphatic channel bringing about growing. The most affected area is the legs due to the dependent part of the body but may be seen in the breast, arm, and genitalia sometimes. It is not obvious to give signs and symptoms immediately after affecting by parasites, it can be shown after a long time as the response of the body's immunity system.
Filarial contamination can likewise cause tropical pneumonic eosinophilia disorder, though this condition is ordinarily found in people living with the infection in Asia. Eosinophilia is the presence of higher than ordinary infection battling white platelets in the body. Side effects of tropical aspiratory eosinophilia disorder incorporate hack, windedness, and wheezing.
Etiology / Causation
It is caused by 3 filarial species:
Brugia malayi
Brugia timori
Wuchereria bancrofti
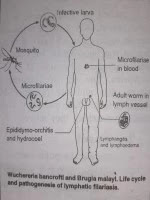
Wuchereria bancrofti is deposited in the lymphatic vessels and gland. The male is about 4 cm by 0.1mm and the female 6cm by 0.2 mm. They copulate, the female becomes gravid, discharging microfilariae (living embryos) into lymphatics, these enter into the bloodstream unless the lymphatics have become occluded by inflammation dye to the primary infection and secondary infection. Microfilariae are found in the peripheral blood at night time in the early stage of infection. Mosquitoes (Culex) are the intermediate hosts in whom microfilariae, sucked during biting, mature into infective larval filariae. They are transferred to human beings through bites by infected mosquitoes, larval filariae inter the lymphatic system, maturing in about 3 months.
Filariasis is common in Central and Eastern India. It also occurs in other countries of South-East Asia and throughout the Pacific region.
Symptoms / Signs
Stage of invasion
The symptoms are mainly allergic taking the form of painful swellings of the scrotum, arms, and legs (like erythema nodosum), urticarial lesions, lymphadenitis, lymphangitis, and filarial fever.
After the adult worms have lodged themselves in lymphatic vessels and glands, the microfilariae are liberated. Only at this stage can they be demonstrated in the peripheral blood. Filarial abscesses, varicose groin glands, lymph scrotum, lymph hydrocele and chyluria, arthritis, etc., are the usual symptoms at this stage. Inguinal and femoral glands are hard and fibrous, when punctured with a syringe, microfilaria can be demonstrated in the lymph. Indurated lymphatics are also seen. In lymph scrotum is enlarged, bulky and itchy. The surface shows lymph varies which on rupture keep on discharging continuously straw-colored fluid.
The most common infestation one comes across is elephantiasis of the legs and scrotum produced by the obstruction of the lymphatic vessels and glands.
There is tense solid edema (which does not pit on the pressure) with furrowed skin. This is usually preceded or accompanied by the repeated attacks of lymphangitis and eosinophilia. Elephantiasis is a very distressing symptom, it often cripples the patient. The lymphatic glands in the groin are often enlarged. Microfilariae are absent from blood at this stage
Diagnosis / Investigation
Demonstration of microfilariae in the night blood.
Eosinophilia, complement fixation, and skin tests.
Diagnosing dynamic contamination is the infectious disease of microfilariae in a blood smear by microscopical test. The microfilariae that reason lymphatic filariasis course in the blood around evening time. Blood assortment ought to be done around evening time or night to concur with the presence of the microfilariae, and a thick smear ought to be made and stained with Giemsa or hematoxylin and eosin. For expanded affectability, focus strategies can be utilized.
Serologic strategies give an option in contrast to infinitesimal recognition of microfilariae for the determination of lymphatic filariasis. The patients, who have filariasis, raised degrees of anti-filarial IgG4 in the blood on a regular basis and these can be found through routine examinations.
Though the patient suffers from filariasis and clinically extinguishes a long time after, in-between the test report may come negative.
How to prevent it?
The most ideal approach to lymphatic filariasis is to stay away from mosquito nibbles. The mosquitoes (culex) that convey the minuscule worms as a rule nibble between the long periods of sunset and sunrise.
On the off chance that you live in a space with lymphatic filariasis:
Use mosquito net
Mosquito repellent, though it is not good for health
Must cover the body with a cloth after evening onwards
Another way to deal with counteraction incorporates giving whole networks medication that executes the minuscule worms — and controlling mosquitoes. Yearly mass treatment lessens the degree of microfilariae in the blood and subsequently, decreases transmission of contamination.
Specialists think that lymphatic filariasis, an ignored tropical illness (NTD), can be dispensed with all around the world, and a worldwide mission to wipe out lymphatic filariasis as a general medical condition is in progress. The end procedure depends on the yearly treatment of entire networks with blends of medications that execute the microfilariae. Because of the liberal commitments of these medications by the organizations that make them, countless individuals are being dealt with every year. Since these medications additionally decrease levels of contamination with intestinal worms, advantages of treatment stretch out past lymphatic filariasis. Fruitful missions to dispense with lymphatic filariasis have occurred in China and different nations.
Complications:
Lymphedema:
Lymphedema is non-pitting edema in extremities because of constant irritation and inflammation for a long time of lymphatic vessels.
Lymphedema ordinarily happens in the upper extremities and may include breasts.
The lower extremities are a typical spot for lymphedema due to the dependent parts of the body.
Hydrocele:
Hydrocele was additionally revealed up to 30 cm in distance across because of lymphedema in the genitalia that may prompt bacterial disease.
A few instances of filariasis of the ovary and mesosalpinx may be detailed.
Renal contribution:
Expanded intestinal lymph seepage in renal vessels causes loss of lymph liquid in pee giving it a smooth appearance.
Treatment
Pressure bandages and surgery help the bad case of elephantiasis.
The prevention of filariasis consists of mass treatment of all infected individuals in an area and the eradication of mosquitoes by the use of insecticides in the breeding places.
Homeopathic medicines in different filariasis
Elephantiasis
Hydrocotile, Anacardium, Arsenic album, Silicea(elephantiasis of scrotum)
Hydrocele
Apis Mel(serious inflammation of testes)
Cal. Flour (induration of testes)
Conium (testicles hard and enlarged)
Graphites(testicles swollen and indurated)
Spongia T. (inflammation or swelling of spermatic cord and testicles with pain and tenderness).
Inflammatory fever
Aconite Nap, Belladonna, Bryonia alba
Lymphangitis
Apis Mel, Ars. iodide, Merc. Sol,
Adenitis
Apis M, Belladonna, Iodium, Phytolocca Dec.


Post a Comment